What to Do When Your Patient Has Supraventricular Tachycardia (SVT)
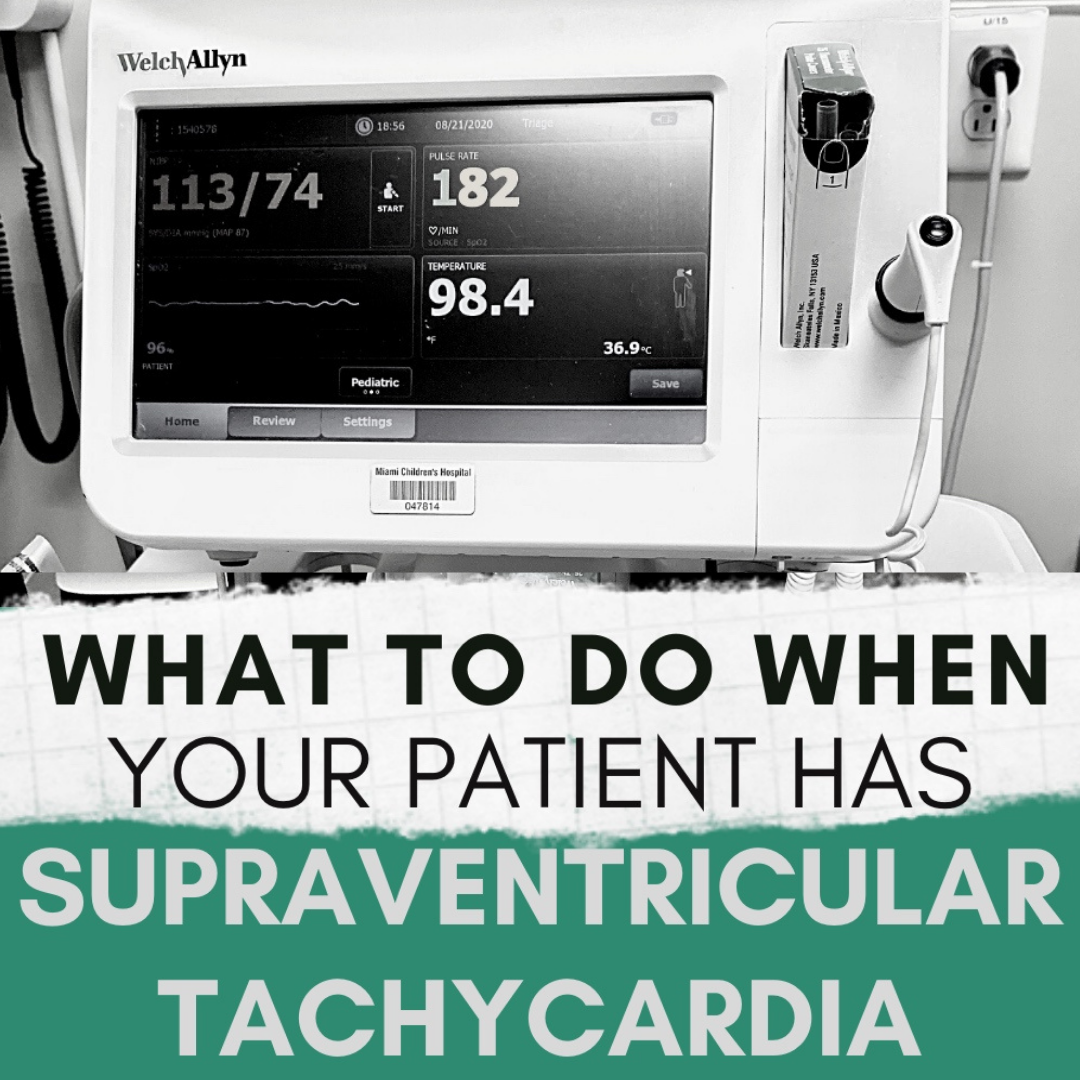
Today we are talkin’ what to do when your patient has Supraventricular Tachycardia. If you’ve ever had a patient with Supraventricular Tachycardia (SVT) you know it can be very worrisome, especially with how fast paced everything becomes after it’s diagnosis. Usually, you identify SVT through an extremely high heart rate and/or patient complaining of palpitations and a racing heart rate. Like all things that are new, unfamiliar and critical, experiencing this as a new nurse can be scary and feel like one of those moments when you might just *freeze* but don’t worry! We have all felt this way at one point or another and I am going to teach you what to do when your patient has Supraventricular Tachycardia, what you need to know to be prepared and avoid that instinct to flight. Let’s jump into it…
What to know about SVT?
Supraventricular Tachycardia (SVT) is an abnormal heart rhythm or arrhythmia defined by its severely increased heart rate. SVT can be symptomatic (where patient is showing s/s of distress) or asymptomatic (patient can be completely calm with no physical symptoms at all).
What defines SVT?
In infants, a heart rate >220 is defined as SVT while a heart rate >180 is definitive in children. Do not confuse Sinus Tachycardia and Supraventricular Tachycardia. These are two different rhythms that require different treatments and interventions.
As mentioned above, SVT can be symptomatic or asymptomatic. Patient’s who are symptomatic may experience:
- Feelings of fluttering heart, palpitations, “racing heart”
- Lightheaded, dizziness, syncope, sweating
- Shortness of breath
How does SVT look on an EKG?
An SVT heart rhythm will appear as the image above. It is important to note that in an SVT rhythm you will have a missing or abnormal P wave. This is because the heart is beating SO fast that the EKG can barely even capture the P wave. Let’s look at a normal sinus rhythm (NSR) or normal heart rhythm compared to an SVT rhythm.


Source: Life in the Fast Lane, https://litfl.com/supraventricular-tachycardia-svt-ecg-library/
As you can see, in our NSR you have your p wave, QRS complex, followed by a t wave. The p wave is completely missing or abnormal in our SVT rhythm.
What to do?
So, what do you do when your patient has supraventricular tachycardia?
EKG.
If a patient comes in complaining of chest pain, tightness in chest, heart palpitations, racing heart, dizziness or any cardiac related symptoms an EKG is most guaranteed. Once an EKG is complete you will be able to detect an SVT rhythm but what about when a child or infant is asymptomatic from obvious physical symptoms and cannot tell you what they feel? Two scenarios usually go down in this case — 1. A parent will tell you they feel their child’s heart racing through their chest or 2. You will immediately detect an abnormal heart rate through your intake vitals check. Usually this heart rate will read VERY high (as mentioned above, over 180). It will alarm you and you will want to recheck it. When you recheck, HR is still extremely elevated. You will immediately call the provider and an EKG will be ordered. If a patient is suspected of having SVT you will:
Provide oxygen and ventilation as needed.
If a patient is experiencing shortness of breath, dyspnea, or oxygen levels are affected you will provide oxygen. Even if SpO2 isn’t affected but the patient is having shortness of breath you will still provide supplemental oxygen to help the patient breathe easily and to lessen the workload of the heart. Remember, when your heart beats it is pumping oxygen filled blood to the rest of your body. If your heart is beating too quickly, it is working harder to oxygenate. Providing supplemental oxygen will give your heart the extra help it needs during an SVT arrhythmia.
Place patient on a continuous cardiac monitor.
A patient with any abnormal heart rhythm must be monitored closely and continuously. You want to make sure the patient does not worsen but also ensure the patient is responding to treatment.
Obtain a PIV immediately and prepare to administer Adenosine.
If possible, obtain an IV or IO immediately. This patient will likely need Adenosine. Adenosine is the medication that treats SVT by bringing down the heart rate. Because of its very short half life, it is critical to place a Peripheral IV (PIV) as close to the heart as possible. Therefore, your location of choice for a PIV would be the Antecubital fossa or AC. This is so the medication can reach the heart as fast as possible and actually have an effect (if you guys are interested, I can make a post all about Adenosine on our Medication Monday’s! Let me know in the comments below).
Attempt vagal maneuvers if possible, but do not delay treatment if patient is hemodynamically unstable.
Vagal maneuvers are techniques that help bring down heart rate naturally. These maneuvers include:
- Valsalva maneuver
- Bearing down as if you were having a bowel movement
- Blowing through a straw, a balloon, blowing out a “birthday candle”
- You can tell kids to pretend a piece of paper is a birthday candle and to blow it out as hard as they can. This helps keep it “fun” for them. Remember, this situation is already scary to begin with. As nurses, aside from acting quickly and responding adequately to this medical emergency, you also need to remember your patient is scared and you are there to calm them down and help them feel safe. We don’t want children to be traumatized by doctors or experiences.
- Applying an icepack to the face
- This is especially used for infants or children who cannot understand how to perform a vasovagal maneuver.
Grab crash cart and prepare for cardioversion.
A patient in SVT will more than likely require cardioversion. Yes, patients can get out of an SVT rhythm via the vasovagal maneuvers or adenosine but if not, you must cardiovert.
As of 2020,
Initial cardioversion: 0.5J – 1J/kg
If patient requires a second cardiovert, up dose to: 2J/kg
Patient is usually sedated for this procedure as it can be painful. When cardioverting you are essentially jolting or shocking the heart at a very price moment during the rhythm and “snapping it out” of its current arrhythmia in hopes to bring it back to normal sinus (if you want a post on cardioversion, let me know in the comments below!).
I hope this helped all of you newer nurses and future nurses on what to do when your patient is having Supraventricular Tachycardia. Always remember, try your best to stay calm and level-headed during an emergency situation. I know it’s easy to say and hard to do, especially in the beginning but I am a true believer that preparation is what helps you stay calm. If you study this you will feel comfortable (or at least calmer) in a situation like this because you will know what to do. When you know what to do, you feel like you have more control and feeling more in control helps you feel like you have a good grip on the situation.
Have you experienced any emergency situation when you felt scared or nervous? How did you overcome it? Looking back now, have you grown from that experience? I bet you have! Comment below.
’till next time,
The RN Educator
Disclaimer: This post is not intended as medical advice and is only to be used as educational and informative content. If you are concerned of any medical issues, please consult your doctor.
Share this:
Related Posts
What’s in a Pediatric Crash Cart? Nursing Students read NOW!
A pediatric crash cart is a mobile unit containing essential equipment and medications required for…